The early detection of breast cancer has reached a significant milestone thanks to an innovative study that combines the power of Artificial Intelligence (AI) with advanced machine learning techniques. Researchers from Massachusetts General Hospital and the Massachusetts Institute of Technology's Computer Science and Artificial Intelligence Laboratory (MIT CSAIL) have developed a predictive model that can anticipate, up to five years in advance, the risk of a patient developing breast cancer. This breakthrough not only represents a major advancement in medical technology but also offers new hope for thousands of women worldwide.
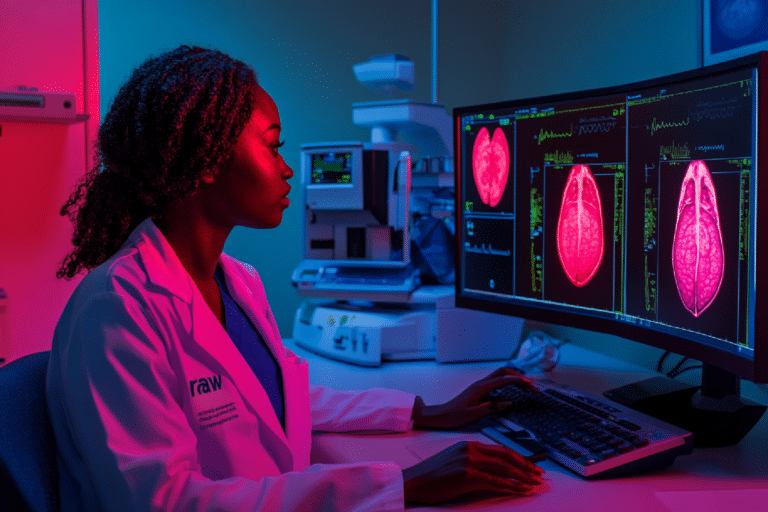
The model in question is based on deep learning technology, an AI approach that simulates how the human brain processes information, allowing the system to learn and improve over time. To train this model, the researchers used a vast dataset consisting of mammograms from 60,000 patients. All these patients developed breast cancer within five years of their initial evaluation. This approach allowed the model to identify subtle patterns in breast tissue—patterns that might go unnoticed by the human eye but are indicative of potential future malignancy.
The model's accuracy is remarkable. With a success rate of 31%, it nearly doubles the effectiveness of conventional diagnostic techniques. This level of precision is particularly relevant in a field where early detection is crucial for the successful treatment of breast cancer. By identifying at-risk patients in advance, doctors can intervene more quickly, offering more effective and personalized treatments.
Comprehensive and Personalized Risk Assessment
One of the most revolutionary aspects of this new model is its ability to provide a more comprehensive and personalized risk assessment. Dr. Constance Lehman, a leading specialist at Massachusetts General Hospital and a professor at Harvard University, has pointed out that the patterns detected in the mammograms not only reflect the likelihood of developing cancer but also capture the influence of various factors. These include genetic predisposition, hormone levels, pregnancy and breastfeeding history, diet, and changes in body weight. This ability to consider multiple variables allows for a much more accurate and tailored assessment for each patient.
Moreover, this personalized approach could be especially beneficial in preventing breast cancer in populations that have historically been underserved or misdiagnosed. The new model has proven to be equally effective across different ethnic groups, overcoming one of the major limitations of current methods. In many cases, traditional diagnostic techniques have shown greater effectiveness in Caucasian patients compared to African American patients, a disparity this new AI model seeks to correct.
The potential impact of this breakthrough cannot be overstated. In the fight against breast cancer, early detection is one of the most critical factors for improving survival rates. This new AI model could radically change how breast cancer detection and treatment are approached, allowing patients and doctors to make informed decisions much earlier.
By providing a longer window of time for intervention, this model could reduce the need for aggressive and costly treatments such as chemotherapy and radiation, which often have significant side effects. Instead, patients could benefit from earlier and less invasive treatment strategies, improving not only their prognosis but also their quality of life.